Understanding Your Treatment Options
Surgery
Click here to learn more about thyroid surgery
Take a moment to learn about thyroid surgery.
What is Surgery?
There are three types of surgery done for MTC, though a combination of them may be completed. Doctors prefer to do only one surgery for MTC to reduce the risk of damage to nerves in the area.
Types of Surgery
Thyroidectomy
Usually MTC is treated with the removal of the thyroid (thyroidectomy). Sometimes only half of the thyroid is removed (thyroid lobectomy), though usually this happens when doctors are unsure if the patient has MTC. If someone has a thyroid lobectomy but then learns he or she has MTC, their doctor may discuss the option of an additional surgery to remove the rest of the thyroid.
Doctors try to save as many parathyroid glands as possible. Sometimes they do this by relocating a parathyroid into the muscle of the neck or arm (autograft), where it will have a healthy supply of blood. Only one working parathyroid gland is needed (out of four) for normal function and normal calcium levels in the blood.
Doctors also try to protect the recurrent laryngeal nerve (RLN) during a thyroidectomy, which protects the patient’s voice. Most of the time, the RLN is not bothered during surgery and functions like normal. However, 4% of patients may have temporary bruising and may become hoarse while their nerve is healing. In 1% of patients, the nerve is permanent injured and they experience permanent hoarseness. For a very small number of patients (1 in 10,000), injury or bruising to their nerves can require a temporary or permanent tracheostomy (a breathing tube through the neck).
Central Neck Dissection
Most patients with MTC will have a central neck dissection (CND) along with their thyroidectomy. With a CND, the lymph nodes in the central neck are removed in order to remove any cancer that may have spread to the lymph nodes around the thyroid. Many times with a CND, two of the parathyroid glands are removed as well (complete resection). Risks of CND include a disruption to the blood supply of the parathyroid glands and damage to the recurrent laryngeal nerve (RLN).
Lateral Neck Dissection
Some patients with MTC will have signs of cancer in their lateral neck area. Doctors will perform a lateral neck dissection (LND) for these patients. Nerves in this area may be affected by surgery, such as the vagus nerve (affects the voice), the spinal accessory nerve (allows the shoulders to shrug), and the phrenic nerve (moves the diaphragm up and down during breathing). Another risk with LND is that lymphatic fluid may leak, causing fluid to accumulate in the neck and sometimes the chest.
Questions to Consider
If you think you may want to choose surgery, you should think about:
- How comfortable am I with the risks of surgery?
- How important is it to me to have a doctor who has done many surgeries for MTC?
- What is the recovery from surgery like?
- Can I recover from surgery at home?
- How often do I need to follow-up with my doctor after surgery?
Active Surveillance
What is Active Surveillance?
Active surveillance is also called observation or long-term monitoring. With active surveillance, people with MTC are watched to see if the cancer is stable, growing, or spreading to other parts of the body. Active surveillance may be done differently person-to-person based on the characteristics of their cancer.
What does the treatment consist of?
Monitoring usually involves visits that include:
- Imaging tests, such as MRIs, CT scans, dotatate scans, ultrasounds and bone scans;
- Lab tests; and
- Physical exams
What are the side effects?
The side effects related to active surveillance are relatively limited and may include:
- Anxiety. An individual could experience unease by feeling that the treatment is too passive and they should be doing something more than observing. This feeling should be discussed with their care team.
- Risks secondary to imaging. In some instances, patients will need long-term repeat imaging that involves ionizing radiation, such as CTs, which over time could have risks for developing other cancers. Care teams should consider this in their treatment plans.
Questions to Consider
- How comfortable you are with observation?
- How often you will need to have tests and exams?
- Where you will need to have tests and exams performed?
Approved Systemic Therapy
What is Approved Systemic Therapy?
Systemic therapy is a type of therapy that treats wherever the disease may have spread in the entire body because it is carried by the blood to those areas. Systemic therapy for MTC is currently given as pills by mouth. “Approved therapies” are systemic therapies that are approved by the Food and Drug administraton (FDA) and considered “standard of care”.
What Does this Treatment Consist of?
Right now, four drugs are approved for MTC:
- Vandetanib (Brand name: Caprelsa), Approved in 2012
- Cabozantinib (Brand name: Cometriq), Approved in 2012
- Selpercatinib (Brand name: Retevmo), Approved in 2020
- Pralsetinib (Brand name: Gavreto), Approved in 2020
Vandetanib and cabozantinib are multikinase inhibitors (MKIs). They target various proteins that cause uncontrolled cell growth.
Selpercatinib and pralsetinib are RET-inhibitors. Patients who have RET mutations can take these drugs.
These drugs can work either by shrinking the cancer or slowing its growth. Patients stay on these drugs as long as the drug is working and they are tolerating it well. These drugs do not help patients live longer or cure their cancer, but they can prevent complications from cancer growth.
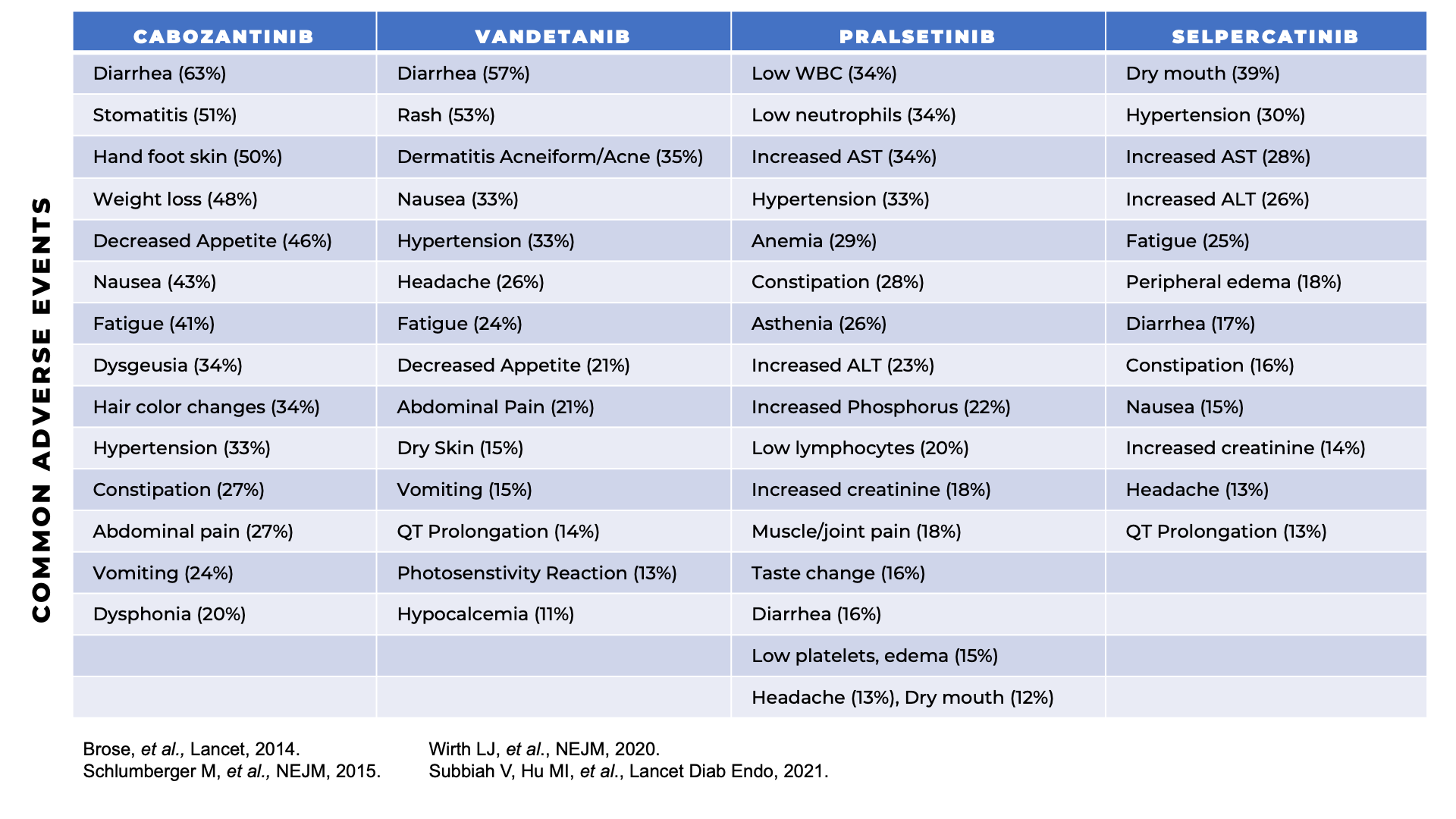
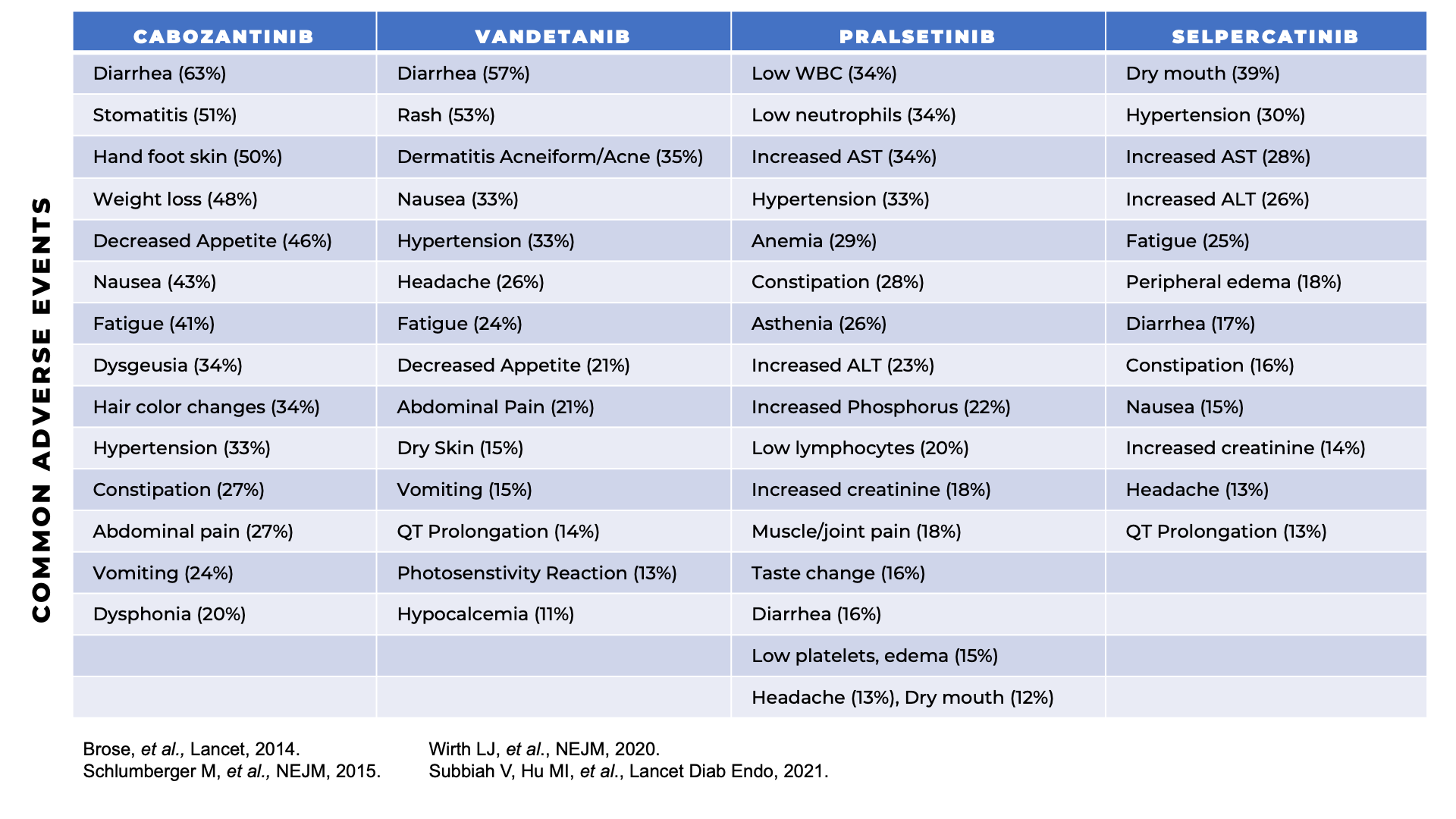
What are the Side Effects?
Side effects vary depending on what drug is used and which dose is used (please see side effects here). Many of the side effects are manageable with either preventive measures, recommendations to take over-the-counter or prescriptive medications, lifestyle and dietary modifications or with dose reduction of the systemic therapy. Routine monitoring of blood pressure, heart rate, weight, and laboratory tests are needed while on systemic therapy to ensure no other side effects develop. Occasionally, your physician will also perform EKGs or echocardiograms to assess for heart function. Referrals to dermatology or ophthalmology may be needed to address other potential side effects.
Questions to Consider
- How frequently I would have to have follow-up appointments?
- Where I would have follow-up appointments?
- What would the side effects be like?
- How long do I need to be on the drug?
Clinical Trials of Systemic Therapy
What Are Clinical Trials of Systemic Therapies?
People whose cancer grows or spreads while using approved treatments may be referred to clinical trials. Clinical trials are research studies that can find new, better ways to treat cancer. These treatments have not yet been proven to have benefits and cannot be given outside of a clinical trial. They must be taken according to strict study-related schedules. Systemic therapy is a type of therapy that treats wherever the disease may have spread. For MTC, systemic therapy can be pills taken by mouth and/or intravenous infusions.
How are Clinical Trials of Systemic Therapy Conducted?
Clinical trials are conducted in 3 phases:
- Phase I: either the drug is used for the first time in a group of patients or it is used in combination with another drug. The purpose is to study the safety of the drug(s) and to identify a dose that patients can tolerate. There is no placebo in this phase of a drug trial.
- Phase II: The drug(s) is used for more patients to study if the drug is an effective treatment. Typically, there is no placebo in this phase. Phase II trials usually enroll a small group of patients (fewer than 50).
- Phase III: The drug(s) is used in a group of patients and is compared with another drug (typically one that is the standard of care) or to a placebo. The purpose of the study is to study whether the study drug is better or as good as the comparator drug. Typically, this study enrolls many patients (more than 100).
There are various ongoing clinical trials for MTC. Your doctor can help you learn more about the clinical trials that are available for you. Information can also be found at clinicaltrials.gov.
To learn more about clinical trials click here.
What Does this Therapy Consist of?
While each specific trial is unique, you can expect some things to be common among most trials. Trials are usually available at specific approved locations and may or may not be available through your current care provider. You usually have to meet pre-defined criteria to be a part of a trial and have to agree to follow the rules of the trial, including schedule of follow up and monitoring methods.
Questions to Consider
- How frequently I would have to have follow-up appointments?
- Where I would have follow-up appointments?
- What would the side effects be like?
- How long do I need to be on the drug?
- How comfortable am I with uncertainty of treatment benefits?
- Who pays for the drug or the study-related costs? Will my insurance pay for me to be on a clinical trial?
- How long will I remain on the clinical trial?
Focal Therapy
What is Focal Therapy?
Focal therapy is a type of treatment that targets disease that is localized to a specific area of the body. Its goal is to shrink or kill cancer that has come back or spread to that specific area to prevent local destruction, pain or complications in the future. Focal therapy is often used when someone’s cancer grows in or near important body parts (e.g. bones or lungs when near the airway).
Types of Focal Therapy
Antiresorptive therapies (zoledronic acid and denosumab) are given intravenously or subcutaneously. They target the bones to make them stronger and to prevent fractures or pain. They may also prevent further cancer spread to their bones. Antiresorptive therapies can be used in combination with surgery and systemic therapy. They may be given once a month, once every 3-4 months or once every 6 months.
Radiation therapy
Radiation therapy uses focused, high-energy photon beams to destroy cancer cells in a particular area of the body, such as the spine. It can be used as a stand-alone treatment or in combination with other therapies. Radiation therapy consists of External Beam Radiation Therapy (EBRT), Stereotactic radiosurgery (SRS), Stereotactic body radiation therapy (SBRT), and proton therapy. Radiation therapy requires careful planning to make sure the tumor is targeted with the smallest impact on the nearby tissues.
Questions to Consider
If you think you may want to choose focal therapy, you should think about:
- What are the possible side effects of focal therapy?
- Will focal therapy control disease elsewhere in my body?
- How frequently would I have follow-up appointments?
- Where would I have follow-up appointments?
- Can I get focal therapy closer to home?
- How long can I expect to be on focal therapy?
- Can I use focal therapy in combination with another treatment?
- Will my insurance pay for this treatment?
- What are the possible side effects of focal therapy?
- Will it control disease elsewhere in my body?
- How frequently would I have follow-up appointments?
- Where would I have follow-up appointments?
- Can I get focal therapy closer to home?










 So far I have learned that there is no room for second-guessing. Go forth and gather the best information to make the best decisions (regarding treatment) and move on. Do not look back. And never ask yourself, "Should I have...?" or "What if?"
So far I have learned that there is no room for second-guessing. Go forth and gather the best information to make the best decisions (regarding treatment) and move on. Do not look back. And never ask yourself, "Should I have...?" or "What if?"





