Questions you may have about Medullary Thyroid Cancer
Understanding the Disease
What is calcitonin, and what role does it play in MTC?
How are calcitonin levels used?
What is Calcitonin Doubling Time (CDT), how is it calculated, and how is it used?
Calcitonin doubling time is the amount of time (usually in either months or years) that it takes for a patient’s calcitonin to double in amount. It is calculated using levels of calcitonin in the blood over multiple time points, usually using no less than two years of levels to calculate. The shorter the doubling time, often the faster the MTC is thought to be growing. Of note, calcitonins should only be used in CDT or compared to one another if they were performed at the same lab.
What factors can affect my calcitonin levels?
Does my calcitonin level correlate with the amount of disease I have?
Typically, calcitonin level does correlate with extent of disease where, when calcitonin is over 500, there is a higher chance that there is disease outside of the neck like lungs, liver, or bones. However, there are times when the medullary thyroid cancer does not produce calcitonin effectively, in which case the calcitonin may seem lower even in the setting of distant metastasis. In this situation, we also look at the CEA level which is typically much lower than the calcitonin level, but if the CEA is somewhat similar to the calcitonin level, that might suggest a dedifferentiated MTC. The higher the calcitonin level, usually the more disease is present.
What is CEA, and what does it mean for an MTC patient?
How do I know the “Stage” of my MTC?
Stage is determined by the extent of disease seen on imaging and pathology. Your physician should be able to tell you your stage of disease.
Staging is described through the TNM classification system and is made up of looking at the primary tumor (described as the T), whether the disease has spread to the lymph nodes (described as the N), and whether the cancer has spread to distant parts of the body (described as M).
Does MTC treatment differ by stage?
What is an MTC Center of Excellence?
A “center of excellence” is an institution that has health care providers with extensive experience in treating MTC. There is not a certification for an MTC center of excellence; however, it is a place that treats a high number of patients with this rare disease.
What kind of health care provider should I see for MTC?
Can MTC be prevented?
Will I ever be considered cured?
Patients are considered cured if they have no evidence of disease on imaging or in evaluation of the tumor markers in their blood. However, we continue to follow such patients because recurrence is always possible in the future.
Other Questions to Ask Your Doctor
- What type of thyroid cancer do I have?
- Who will be part of my health care team, and what does each member do?
- How do individuals in training fit into my care?
- What is the best way for me to remain in contact with my care team?
- Can you explain my pathology report, imaging, or laboratory test results to me?
Genetics
Why should I consider genetic testing and/or counseling?
To find a genetic counselor in your area, you can visit https://findageneticcounselor.nsgc.org
Why would I be tested for pheochromocytoma/and or primary hyperparathyroidism? Do I need to get a blood or urine test for this?
If a patient has an RET gene mutation/change that causes hereditary medullary thyroid cancer, they also are at risk for developing pheochromocytoma and primary hyperparathyroidism. Therefore, they would be tested annually for these two diseases. Usually this testing is a blood test but sometimes can be a urine test.
What is the difference between germline and somatic mutations?
All tumors and cancer are caused by changes in genes. These changes are called mutations. In patients with an inherited disease like MEN2, the disease-causing mutation is in every cell of the body when they are born, and this is called a germline mutation. Sometimes mutations occur only within the tumor or cancer itself. These mutations are called somatic mutations and are acquired over time. Somatic mutations are not present from birth nor can they be passed down to the next generation. Germline mutations are typically detected through a blood or saliva test, while somatic mutations are detected by evaluation of the tumor tissue itself.
If I have MEN2, does that mean I have MTC too?
Are there ways to prevent passing this mutation to my future children?
25% of MTC is hereditary (runs in families). The first step is to determine whether you have a hereditary cancer syndrome through genetic testing. Individuals with a known hereditary cancer syndrome, such as MEN2, may choose to use preimplantation genetic diagnosis, or PGD, to ensure they won’t pass the hereditary syndrome on to their children. PGD is the process of performing genetic testing on embryos for a known hereditary cancer syndrome and only using embryos that do not have the hereditary syndrome through the process of in-vitro fertilization (IVF).
If I get genetic testing, will this affect my insurance coverage?
Treatment
General Treatment Questions
General Treatment Questions to Ask Your Healthcare Provider
- What are my treatment options?
- What long-term side effects or late effects are possible based on the cancer treatment I received?
- What is the goal of each treatment? Is it to eliminate the cancer, help me feel better, or both?
- Who will be leading my overall treatment?
- What experience do you have in treating this type of thyroid cancer?
- Do I need to make a treatment decision right away?
- What will we do if the treatment doesn’t work or if the cancer recurs?
- Where can I get a second opinion?
Questions About Surgery
Can MTC be treated by surgery?
If thyroid surgery is recommended, how much of my thyroid gland will be removed?
Will lymph nodes be removed as well?
What type of scar can I expect?
How experienced in MTC should the surgeon for this type of surgery be?
In general, improved outcomes have been found in patients seen by surgeons who operate on the thyroid frequently. Because MTC is rare, it is also helpful for the surgeon to have familiarity with MTC specifically.
What tests would I need before surgery?
- A comprehensive neck ultrasound to include the thyroid bed and the lateral neck compartment
- Tumor markers including serum calcitonin and CEA
- Additional imaging based on extent of disease suspected
- Evaluation of vocal folds if there is concern for tumor involvement
Will surgery cause hypothyroidism? If so, how do you treat hypothyroidism?
If your entire thyroid is removed, you will be hypothyroid and will need thyroid hormone replacement in the form of daily medication.
How can I expect to feel differently without my thyroid?
Sometimes patients report feeling some fatigue and experience challenges with weight changes.
Why is preserving the parathyroid during surgery important?
Do I need to get my tissue tested for mutations after initial surgery?
Testing tissue for mutation is usually reserved for when additional therapy is planned for advanced diseases.
Will I only have one surgery in my neck for MTC?
Ideally, you would only have one operation within the neck. However, because MTC can recur, additional operations may be necessary. Knowing the diagnosis prior to surgery and performing complete preoperative imaging allows for the best chance of an optimal first surgery.
What can my healthcare team learn from my pathology?
Your team can learn about the extent your disease has spread which can help with staging and determining how the disease will behave.
Do I need to have surgery to understand my disease stage?
Not necessarily, as sometimes imaging can be used to determine if there is disease in the lymph nodes in the neck, and it is often used to determine if there is disease that has spread elsewhere in the body.
See How do I know the “Stage” of my MTC? in the Understanding the Disease section above for more information about MTC staging
What are potential common complications of surgery?
Questions About Hormone Replacement Therapy
When do I need to start taking thyroid hormone pills? If so, for how long?
If I need to take thyroid hormone replacement, how often do I need my dose checked through blood tests?
If I miss a dose, will that affect me in the long term?
What situations can interfere with thyroid hormone replacement?
In addition, diarrhea which can be problematic in MTC patients can alter the absorption of thyroid hormone into the body and require higher doses.
Other Hormone Replacement Therapy Questions to Ask Your Healthcare Provider
- Who should I contact about any side effects of hyperthyroidism or hypothyroidism I experience? And how long should I wait?
- Will my dose be adjusted in the future? How often?
- Do I need to take my thyroid hormone at the same time daily?
Questions About Systemic Therapy
When do I need to be placed on systemic therapy?
What medications are currently approved for the treatment of MTC in the United States?
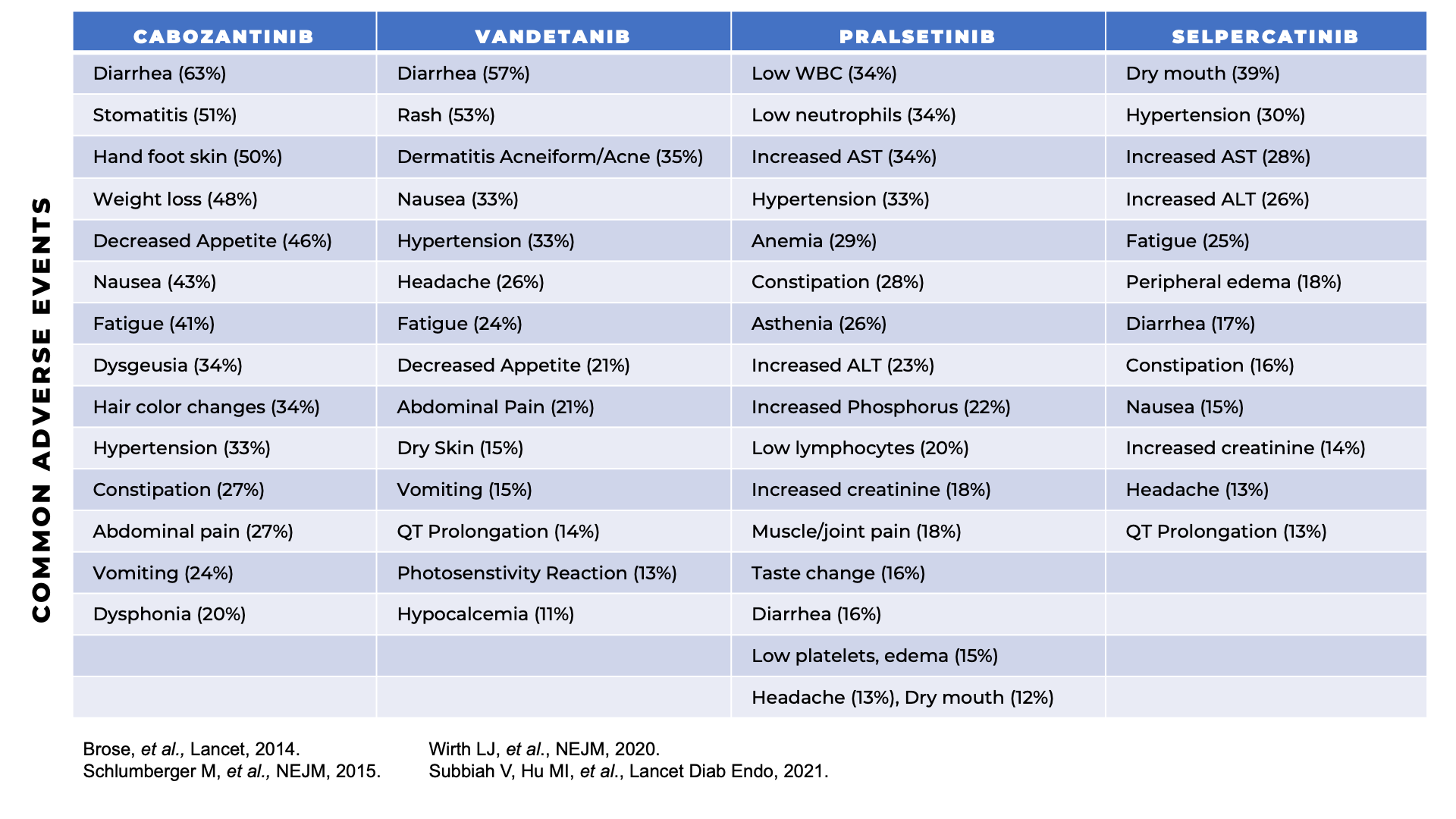
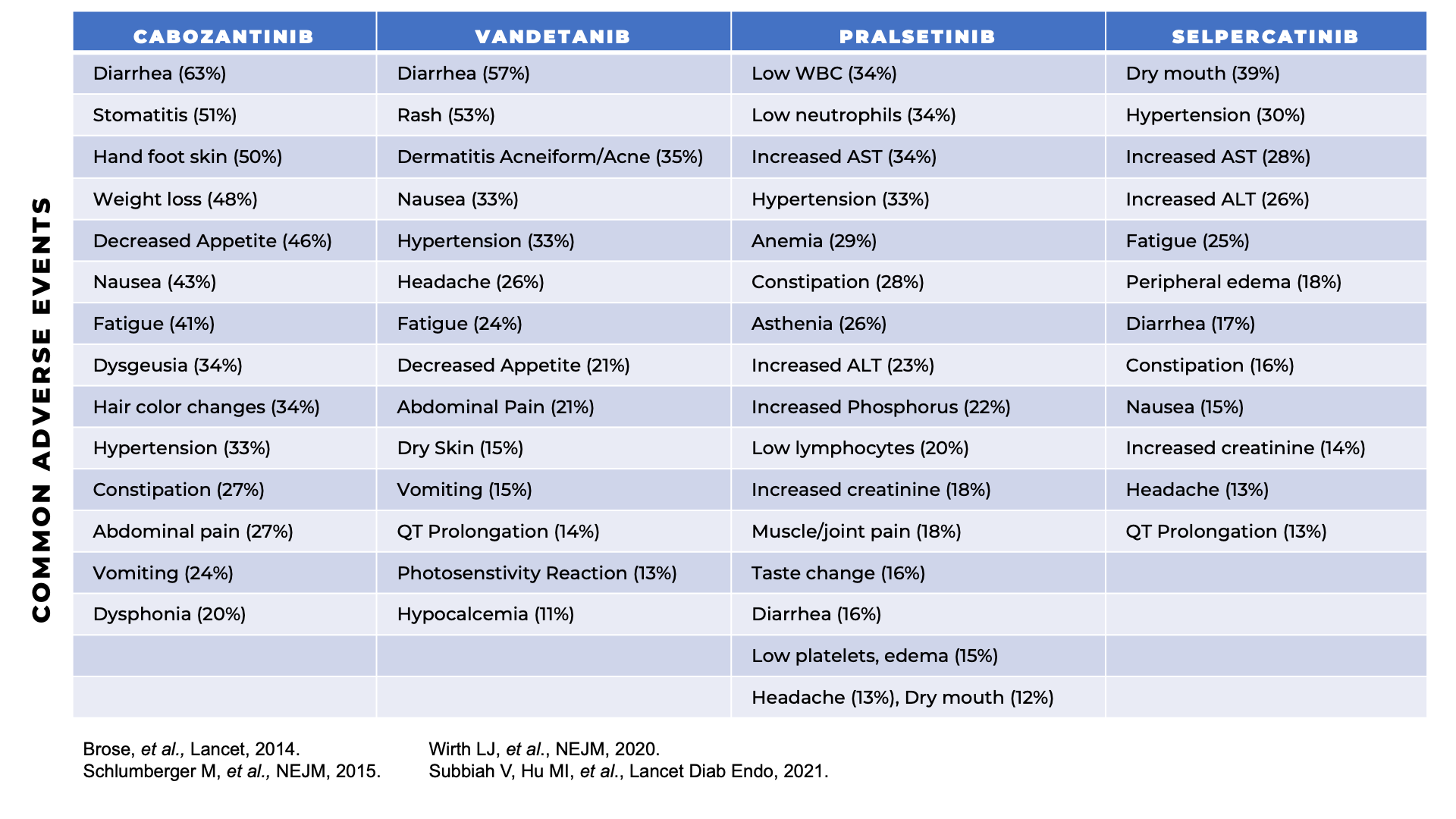
Vandetanib, Cabozantinib, Selpercatinib, and Pralsetinib have been approved by the Food and Drug Administration (FDA) for the treatment of MTC in the United States.
What clinical trials are available? Where are they located, and how do I find out more about them?
Other Systemic Therapy Questions to Ask Your Healthcare Provider
- Should I think about taking part in a clinical trial?
- If I am on a clinical trial, can I complete the requirements locally?
- What should I do to be ready for treatment?
- What are some ways I can remind myself to take my pill each day?
- What long-term side effects or late effects are possible based on the systemic treatment I receive?
- Whom should I contact about any side effects I experience? And how long should I wait?
- What is the chance that I will have to stop taking the drug due to side effects? What can be done to monitor and relieve the side effects?
- Will there be dose changes while I’m on this drug?
Questions About Radiation
How does radioactive iodine differ from radiation treatment?
Is radioactive iodine treatment recommended?
Radioactive iodine is not recommended for MTC as medullary thyroid cancer cells do not have iodine receptors and will not absorb the radioactivity and be treated by it.
In what locations of the body is radiation recommended?
At times, external beam radiation may be recommended to areas of focal progression, such as a bone metastasis or a lung metastasis that is near an airway. Rarely, if there is invasive disease in the neck involving the wall of the trachea or the esophagus, radiation may be recommended for focal treatment to prevent progression in that region in the future. However, external beam radiation therapy to the neck must be considered with significant caution and only after discussion in a multidisciplinary fashion, as radiation to the neck can lead to serious side effects, as well as limit or prevent future beneficial surgery in the neck.
Radiation Questions to Ask Your Healthcare Provider
- Whom should I contact about any side effects I experience? And how soon?
Questions About “Watch and Wait” or Active Monitoring
What is “watch and wait” or active monitoring?
Does watching and waiting mean my disease is not being treated?
What is the chance that the cancer will come back? Should I watch for specific signs or symptoms?
Often, MTC may lead to no symptoms. If there are symptoms, the most common ones are diarrhea or facial flushing. If you develop any of the following symptoms, it may suggest recurrent disease: swallowing problems, new voice changes, or back pain.
Question to Ask Your Healthcare Provider About “Watch and Wait”?
- How will we know if the cancer has come back? What should I watch for?
Questions About Follow-up Care
Question to Ask Your Healthcare Provider About Follow-Up Care?
- What follow-up tests will I need, and how often will I need them?
- Will I need to stop taking thyroid hormone replacement for these tests? If so, for how long and what can I expect during this time
- How do I get a treatment summary and survivorship care plan to keep in my personal records?
- Who will be leading my follow-up care?
- What survivorship support services are available to me? To my family?
Questions About Quality of Life
Question to Ask Your Healthcare Provider About Quality of Life?
- How will this treatment affect my daily life? Will I be able to work, exercise, or perform my usual activities?
- Could this treatment affect my ability to become pregnant or have children? If so, should I talk with a fertility specialist before cancer treatment begins?
- If I’m worried about the costs of cancer care, who can help me?
- What support services are available to me? To my family?
- What would be the limitations after work?
- What is my life expectancy with MTC?
- What is my chance of a full recovery?
 So far I have learned that there is no room for second-guessing. Go forth and gather the best information to make the best decisions (regarding treatment) and move on. Do not look back. And never ask yourself, "Should I have...?" or "What if?"
So far I have learned that there is no room for second-guessing. Go forth and gather the best information to make the best decisions (regarding treatment) and move on. Do not look back. And never ask yourself, "Should I have...?" or "What if?"















